Introduction
The roots of the term “ceramic” can be traced back to the Greek word “keramos”, meaning “pottery”. Keramos in turn is derived from a Sanskrit origin, meaning “to burn”. Thus, it may be reasoned that a ceramic material is a substance that is tempered through burning or heat-treating. A more scientific definition of the word “ceramic” would be a material that contains both metallic and non-metallic elements held together by strong ionic and covalent atomic bonds.
In modern times, ceramics are a widely used group of materials utilized in different fields of technology such as electronics, telecommunication, aeronautics and medicine, among others. The versatile use of ceramics can be attributed to their diverse mechanical, optical and conductive properties that depend on their chemical composition. Independent of the chemical elements used, however, a ceramic material can exist in an amorphous, crystalline or polycrystalline form, as well as mixtures thereof. The amorphous phase shows no crystal growth and is therefore optically translucent but mechanically weak. In contrast, the polycrystalline phase is characterized by a large number of crystals of different sizes, which renders the material strong, brittle and opaque.
In dentistry, ceramic materials can be employed for the reconstruction of highly esthetic areas as well as a framework material for long-span restorations, and almost everything in between. To select a suitable restorative material for a given clinical indication, it is important for the clinician to understand certain innate properties of a ceramic material, such as the flexural strength (in megapascal MPa), fracture toughness (KIc, in MPa x m1/2) and elastic modulus (in gigapascal GPa). Ceramic materials are often employed in dentistry due to their numerous advantages such as resistance to corrosion, chemical inertness and excellent biocompatibility. Furthermore, the possibility to fabricate ceramic restorations through computer-aided design and computer-aided manufacturing (CAD/CAM) renders them cost- and time-effective. On the downside however, the spectrum of ceramics used in implant dentistry is rather large and detailed knowledge of chemical composition, mechanical properties and clinical handling is necessary for an optimal result.
Therefore, this overview article aims to highlight the different classes of ceramic materials currently used in implant dentistry and proposes handling guidelines for both dentist and dental technician.
Silicate ceramics
The largest group of ceramic materials used in dentistry is often called silicate ceramics due to silicon being the central chemical element. Silicon-oxides are very versatile molecules that can be combined with various other elements to form different stones, glasses and crystals. In contrast to glasses, however, dental silicate ceramics are characterized by a controlled crystal growth within the glassy matrix (glass-ceramics). This crystal growth can be modified by mixing different additives to the silicon-oxides, resulting in crystals of different sizes and shapes with distinct parameters. Aluminum, for example, is often added to form crystals such as feldspar or leucite (aluminosilicates). Other notable crystals include fluorapatite, lithium-aluminosilicate and lithium-(di)silicate. The ratio of amorphous glassy matrix and crystal type determines the final optical and mechanical properties of the ceramic material.
Feldspathic ceramic features a high amount of glassy matrix interspersed with a few crystals. The glass phase leads to high translucency and therefore a favorable esthetic appearance, while the decreased percentage of crystals leave the material mechanically weak (flexural strength ~100MPa, toughness KIc~0.9MPa x m1/2). In implant dentistry, feldspathic ceramic is almost exclusively used as a veneering ceramic for stronger framework materials. Veneering remains a manual fabrication step done by the dental technician to achieve an optimal esthetic result for the individual clinical situation. This process also bears potential risks for the introduction of errors or impurities (air bubbles), which may further weaken the material.
Ceramic materials with a higher amount of crystal growth and less matrix generally exhibit stronger mechanical resistance at the cost of some light transmittance. Lithium-(di)silicate reinforced glass-ceramics for example shows a material strength that enables it to be used for monolithic restorations (flexural strength ~350-400MPa, toughness KIc~2-3MPa x m1/2). This type of glass-ceramic is well documented and shows excellent clinical success (Pieger et al 2014; Malament et al 2019). However, the correct manufacturing protocol is essential to ensure optimal surface topography and esthetics. As there are currently no multi-color blanks available, the dental technician has to compensate for the monochromatic base material by applying superficial ceramic staining and glazing. This is almost always necessary to achieve a natural looking and esthetically pleasing restoration. It is generally preferable to select a slightly brighter blank color and then apply chromatic stains in the body and cervical areas of the reconstruction. Another critical aspect is the reduction of surface roughness on the occlusal surface of the reconstruction, as this will otherwise inevitably lead to wear of the antagonist. Therefore, the occlusal surface should be very well polished by applying graduated silicon polishing tools before the final layers of stain and glaze.
Clinical indications for lithium-(di)silicate reinforced glass ceramics include implant-supported single crowns in the anterior and posterior regions as well as short-span fixed dental prostheses (FDP) up to the premolar region. In order to adhesively bond any silicate ceramic material, hydrofluoric acid etching must be used to pre-treat the bonding surface. Furthermore, a coupling agent that contains silane should be applied to achieve optimal chemical fusion to the resin cement.
A clinical case illustration of a monolithic lithium-disilicate implant-supported single crown (Figs 1-4):
Oxide ceramics
Oxide ceramics, sometimes also referred to as high-strength ceramics, are a group of materials that feature almost no glassy matrix, but are comprised almost exclusively of crystals. The base elements in this group are not silica, however, but zirconium or aluminum. In dentistry, the most widely used oxide ceramic is zirconia (zirconium-dioxide), due to its high flexural strength (~1000 – 1200MPa) that surpasses even steel. In contrast to a metal however, zirconia cannot deform under stress and is therefore very brittle (fracture toughness KIc3-8 MPa x m1/2, elastic modulus ~200GPa).
The crystalline form of zirconia can exist in the monoclinic phase (at room temperature), in the tetragonal phase (at ~1170°C) or in the cubic phase (at ~2370°C). In order to stabilize the strong tetragonal phase at room temperature, a stabilizing agent in the form of yttrium or cerium is added. If a crack forms in this metastabilized phase, the stress can lead to a local transformation back to the monoclinic phase. This phase transformation induces a localized volume expansion of around 4% that acts as a counter-pressure and keeps the crack from propagating. This fact makes tetragonal zirconia an ideal material for situations where high strength over a long time period is required, such as frameworks or monolithic restorations. As an alternative to the highly opaque appearance of tetragonal zirconia, manufacturers have recently begun offering zirconia in the cubic phase. While this phase offers better esthetic characteristics due to higher light transmittance, the phase transformation effect is lost which leaves the material mechanically weaker (400 – 800MPa).
Generally, zirconia may be used as a monolithic restoration or as a framework for a bi-layered reconstruction. In the dental laboratory, zirconia is usually milled from a block of pre-crystallized material using CAD/CAM technology and then sintered at high temperature. It is advisable to polish the work piece before sintering to achieve a smooth surface topography. When working with monolithic restorations, a glaze layer should be applied only on the axial surfaces and not on the occlusal area. This is due to the fact that the glaze layer wears off after roughly 6 months of function, leaving potentially unpolished zirconia exposed (Etman, 2009). In order not to endanger the opposing dentition, it is preferable to have an optimally polished occlusal surface of the zirconia reconstruction, minimizing wear. If zirconia is used as a framework, it is critical to choose a veneering ceramic that is compatible with the coefficient of thermal expansion (CTE) of zirconia, which compensates the slower heating and cooling rates.
Clinically, zirconia has been documented to be a successful reconstructive material for many different indications. Implant-retained single crowns and FDPs in both anterior and posterior areas show excellent clinical results (Pjetursson et al. 2018; Sailer et al. 2018; Le et al. 2015). If the esthetic appearance is not critically important, a monolithic reconstruction method is preferred due to fewer technical complications (risk of ceramic chipping is eliminated). When working with FDPs, tetragonal zirconia should be used, either monolithic or buccally veneered. Zirconia may also be used as a framework for full arch restorations. While the results for this reconstruction method seem to be promising, it should be noted that there is currently limited long-term documentation available (Bidra et al, 2017) .
When adhesive bonding to zirconia is desired, acid etching cannot be used to pre-treat the material as there is no silica matrix available. Therefore, in order to achieve an optimal chemical bond to zirconia, the surface must be sandblasted with (silica-coated) aluminum oxide particles of around 30µm in size. If a larger grain size is used, the sandblasting may lead to microcracks, which reduces the mechanical stability. After sandblasting, a coupling agent containing the 10-MDP molecule (10-methacryloyloxy-decyl-dihydrogen-phosphate) must be applied to the bonding surface. Ideally, a cement that also contains the 10-MDP molecule is chosen for optimal adhesive properties.
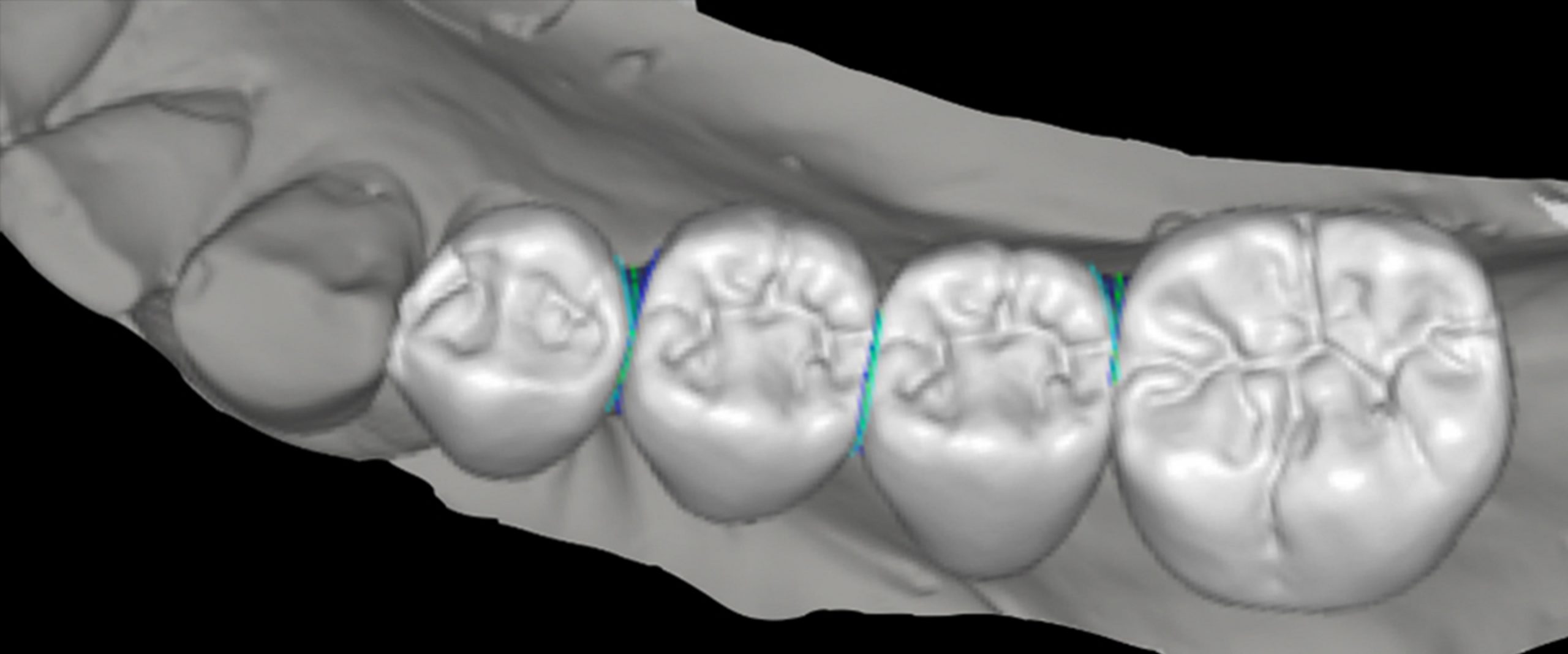
A clinical case illustration of a monolithic zirconia implant-supported FDP (Figs 5-8):
Hybrid ceramics
The continuing development in the field of material science has led to a new class of materials becoming available, often called hybrid ceramics. The term “hybrid” signifies that a ceramic material is combined with another component, usually a polymer (urethane dimethacrylate UDMA/ triethylene glycol dimethacrylate TEGDMA). The purpose of combining these materials is to profit from the strength of a ceramic as well as the elasticity of a resin, thus mimicking natural tooth substance. The ceramic portion (usually feldspathic) can exist either as a structured network or as crystalline filler particles interspersed into a resin matrix. In both cases the flexural strength (~120-180MPa) and fracture toughness (KIc ~1.5MPa x m1/2) lie between a traditional resin composite and glass-ceramics. The low elastic modulus (~25-30GPa) is close to that of natural dentine and allows the hybrid material to act as a shock absorber.
One of the main advantages of a hybrid ceramic material is that no heat treatment is necessary to temper the material. Therefore, a work piece may be milled out of a prefabricated block and directly post-processed (coloring & polishing). This fast fabrication procedure also allows for chairside use of hybrid materials, which constitutes another advantage. On the downside, hybrid ceramics are prone to wear due to their decreased strength and hardness. Another disadvantage seems to be the long-term color stability. The ideal application strategy for hybrid materials is in a chairside workflow, applying multicolor blocks or blanks that already incorporate color gradients. If the desired color is close to the multilayer blank, the milled reconstruction can be directly finalized. Otherwise, a light-curing esthetic staining and glazing system can be applied to individualize the restoration further. In both cases, the final restoration has to be high-gloss polished using graduated silicon polishing tools and a finisher paste containing diamond particles.
Hybrid ceramics are a relatively new restoration material but seem to perform well clinically (Spitznagel et al, 2018; Bustamante-Hernández et al, 2020). They are designed for implant-supported single crowns in the anterior and posterior area. Currently, hybrid ceramics do not offer sufficient mechanical properties for multi-unit restorations. As these hybrid materials contain both ceramic and resin components, either sandblasting or acid etching with hydrofluoric acid can be employed to achieve adhesive bonding. In both cases however, a coupling agent containing silane should be applied onto the bonding surface.
A clinical case illustration of a monolithic hybrid ceramic implant-supported single crown (Figs 9-12):
Veneering ceramic/porcelain-fused-to-metal (PFM)
Traditional metal-ceramic restorations use a metallic framework that provides mechanical stability, combined with a veneering ceramic to improve the esthetic appearance. This restoration method is well documented in the literature and offers excellent clinical success (Pjetursson et al 2018; Sailer et al 2018, Lemos et al 2019). At the same time however, the bi-layered nature of these restorations comes with potential technical complications. Chief among them is the fracture of the veneering ceramic (“chipping”). In recent years, this problem could be somewhat addressed by the development of more optimized veneering ceramics that have a stronger interface to the substrate. Nevertheless, a certain technical sensitivity remains, especially during the manufacturing process in the dental laboratory. Other disadvantages of metal-ceramic restorations include potential intolerances/allergies, the release of metallic ions into the surrounding tissues and a high opacity.
When working with veneering ceramics, it is of critical importance to choose a material that is compatible with the coefficient of thermal expansion (CTE) of the framework material. If the CTE of framework and veneering are not matched, the different heating and cooling behavior during firing may lead to microcracks, thus significantly weakening the material interface. Therefore, a different veneering ceramic may have to be chosen for zirconia, precious alloys and non-precious alloys.
With the advent of digital dentistry, implant-supported metal-ceramic reconstructions can also be fabricated using CAD/CAM technology. This provides frameworks with an excellent fit to the implant interface, while being more time- and cost-efficient than traditional cast fabrication. At the same time however, the manual veneering process performed by the dental technician remains very time intensive. The different laboratory steps such as oxidation, opaquer application and veneering have to be followed precisely, which requires intimate knowledge of this workflow. Furthermore, the veneering ceramic has to be applied over several firing cycles due to ceramic shrinkage. During these fabrication cycles, crack initiations as well as material impurities remain a constant risk. Therefore, the most important drawback of this traditional workflow is its inefficient manual veneering workflow that may even lead to deviations from the planned shapes and contours.
Clinically, veneered metal-ceramic reconstructions are still suitable for many indications. Most notably long-span or full arch reconstructions benefit from the long-term stability that a metallic framework offers. Furthermore, cantilevered restorations or situations where increased shear-forces are present (such as a canine guidance function) may be difficult for a ceramic to withstand and thus a metallic substructure might be preferred.
A clinical case illustration of a veneered cobalt-chromium implant-supported FDP (Figs 13-16):
Conclusion
Ceramics are a versatile restoration material that can be used for many different clinical indications. Knowledge of the chemical composition, mechanical properties, esthetic characteristics and clinical handling are essential for an optimal result. To ensure the correct choice of material, good communication and collaboration with the dental technician is of importance. Nevertheless, ceramics remain a technically sensitive group of materials that require advanced knowledge on the part of both dentist and dental technician.
Learn more: Ceramic materials learning pathway